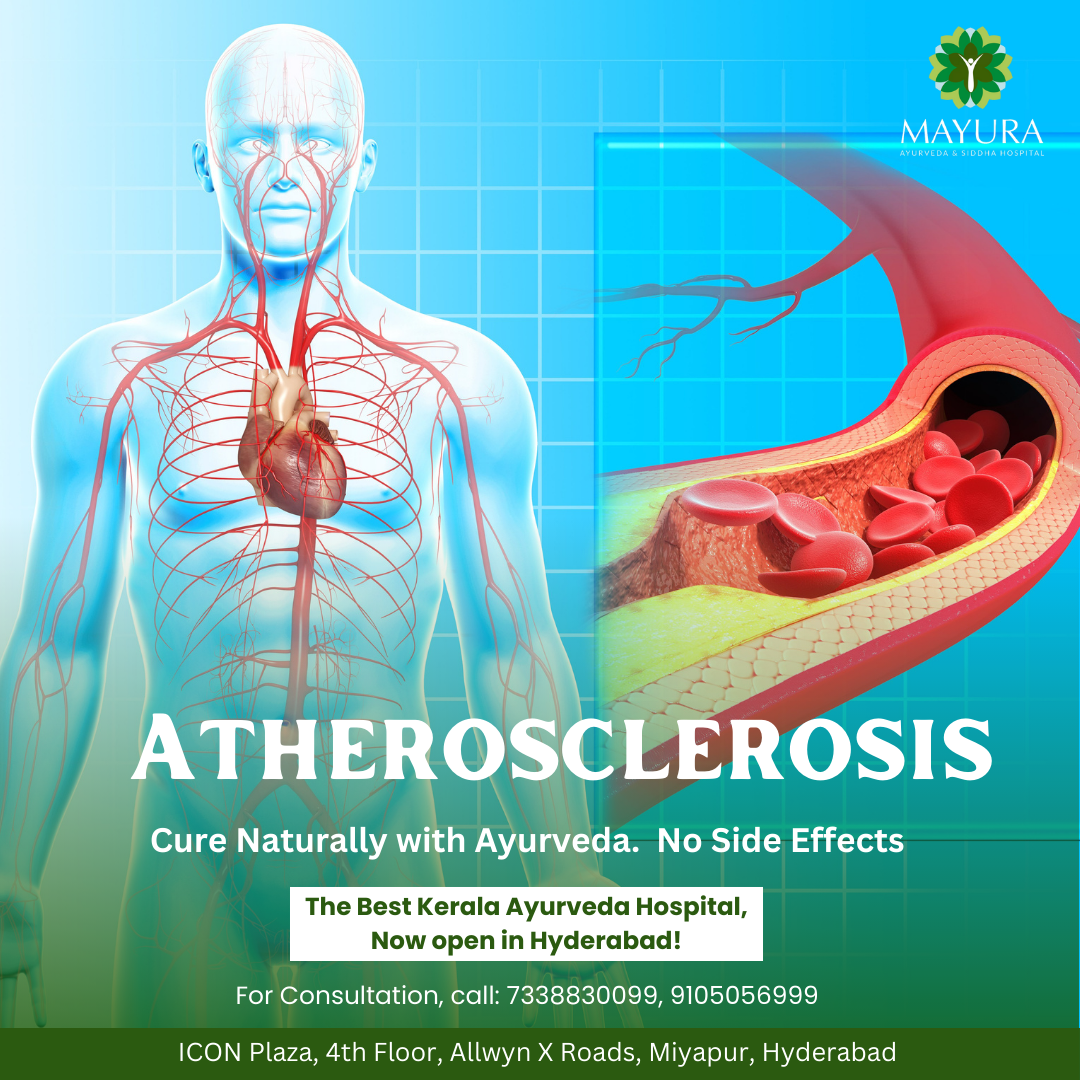
Atherosclerosis stands as a leading cause of cardiovascular disease worldwide, posing significant health risks and challenges. This blog aims to unravel the intricacies of this condition, offering insights into its pathogenesis, clinical manifestations, and contemporary approaches to management.
Understanding Atherosclerosis
At its core, atherosclerosis involves the progressive buildup of plaque within the arterial walls, leading to narrowing and stiffening of blood vessels. This process, driven by a complex interplay of genetic, environmental, and lifestyle factors, contributes to impaired blood flow and heightened risk of cardiovascular events.
Unraveling the Causes
The development of atherosclerosis often begins with endothelial dysfunction, triggered by factors such as high cholesterol levels, hypertension, smoking, diabetes, and inflammation. Over time, these insults promote the deposition of cholesterol, immune cells, and cellular debris, fostering plaque formation and arterial damage.
Recognizing Symptoms
Atherosclerosis may remain asymptomatic for years, silently progressing until complications arise. Common symptoms include chest pain (angina), shortness of breath, fatigue, and weakness. In severe cases, the obstruction of blood flow can precipitate acute events like heart attacks and strokes, necessitating urgent medical attention.
Diagnostic Approaches
Various diagnostic modalities aid in the detection and assessment of atherosclerosis. These include lipid profile tests, imaging studies such as ultrasound and CT angiography, and invasive procedures like coronary angiography. Early detection enables timely intervention and risk stratification to mitigate adverse outcomes.
Management Strategies
The management of atherosclerosis encompasses multifaceted interventions aimed at reducing cardiovascular risk and slowing disease progression. Lifestyle modifications, including dietary changes, regular exercise, smoking cessation, and weight management, form the cornerstone of prevention and treatment efforts.
Pharmacological Interventions
Pharmacotherapy plays a pivotal role in managing atherosclerosis and its associated risk factors. Medications such as statins, antiplatelet agents, blood pressure-lowering drugs, and antidiabetic agents are commonly prescribed to optimize lipid profiles, prevent clot formation, and control hypertension and diabetes.
Interventional Procedures
In cases of advanced atherosclerosis or symptomatic disease, interventional procedures like angioplasty with stent placement or coronary artery bypass grafting (CABG) may be warranted to restore blood flow and alleviate symptoms. These interventions are typically reserved for individuals with significant arterial blockages or those at high risk of adverse events.
Lifestyle Modification Tips
Encouraging patients to adopt heart-healthy habits is paramount in atherosclerosis management. Emphasize the importance of a balanced diet rich in fruits, vegetables, whole grains, and lean proteins, along with regular physical activity and stress management techniques.
Patient Education and Empowerment
Educating patients about the risks associated with atherosclerosis and empowering them to take proactive steps toward prevention and management are essential. Emphasize the significance of medication adherence, regular follow-up visits, and self-monitoring of symptoms to optimize outcomes and enhance quality of life.
Conclusion
Atherosclerosis represents a formidable health challenge with far-reaching implications. By fostering a comprehensive understanding of its underlying mechanisms, recognizing key symptoms, and implementing evidence-based management strategies, healthcare providers can play a pivotal role in combating this pervasive disease and promoting cardiovascular health for all.